Recently funded research
We help paediatric researchers across Children’s Health Queensland raise the bar at a global level through sharing knowledge, discoveries, ideas and innovations.
To date, our funding has supported research in Indigenous health, oncology, nutrition, brain and behaviour health, eye health, cardiovascular and respiratory disease, infection and immunity, oncology and immunotherapy, and emergency and critical care.
Children’s Brain Cancer Centre
Despite advances in other types of childhood cancer, survival rates for brain cancer have made little progress over the past 30 years.
The Children’s Brain Cancer Centre aims to change that. This Centre brings together the ‘best of the best’ in paediatric brain cancer research to bring new hope to children and young people fighting this devastating disease.

Ian Frazer Centre for Children's Immunotherapy Research
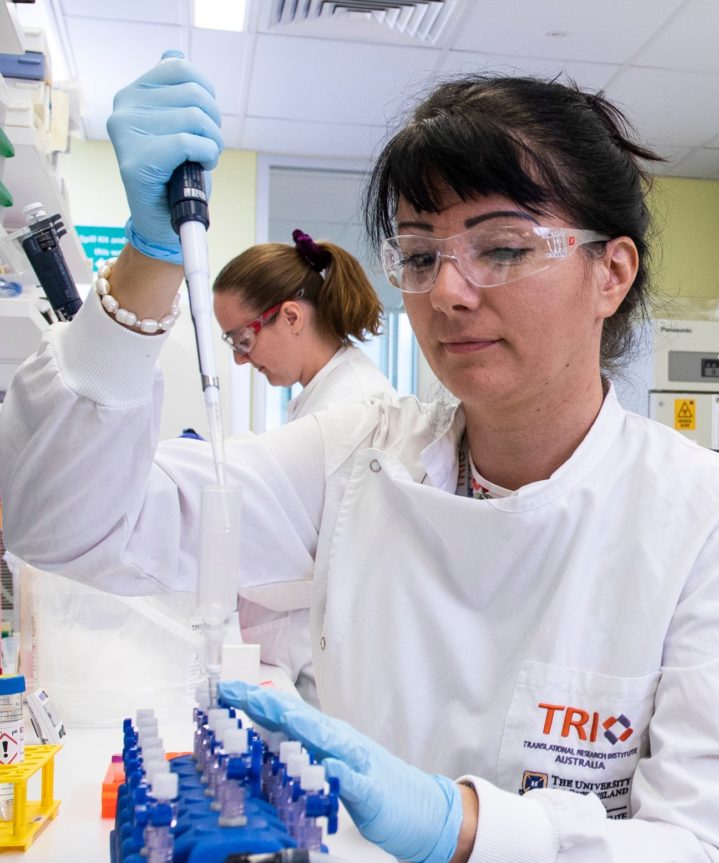
The Ian Frazer Centre for Children’s Immunotherapy Research is the first dedicated children’s immunotherapy research centre in Australia.
By capitalising on the strengths of a multidisciplinary team of experts, the Centre will accelerate the pace of discovery and ensure research is translated into a new era of children’s cancer treatments. The Centre will harness immunotherapy potential to make significant improvements in children’s survival and survivorship.

Our Research Advisory Committee
The Children’s Hospital Foundation is committed to accountability and transparency in awarding funds to paediatric research.
Applications for research funding undergo a rigorous peer-review process conducted by an independent Research Advisory Committee consisting of eminent researchers with broad research experience in preclinical, clinical and health services research.